Billing NC Medicaid PCS PHP Managed Care Organizations (MCOs) in Barnestorm
Overview: The following are basic steps to sending EVV Visit files and creating electronic claims for MCO payers. Note that each section will mention if it pertains to HHAeXchange and/or CareBridge and corresponding MCOs. EVV Visit: EVV Visit in Barnestorm refers to the appropriate documentation for Electronic Visit Verification based on the 21st Century Cures Act. When your agency opts to use Barnestorm as the selected alternate EVV vendor, you agree to use the Care Champ app or telephony to be compliant with the EVV requirements. 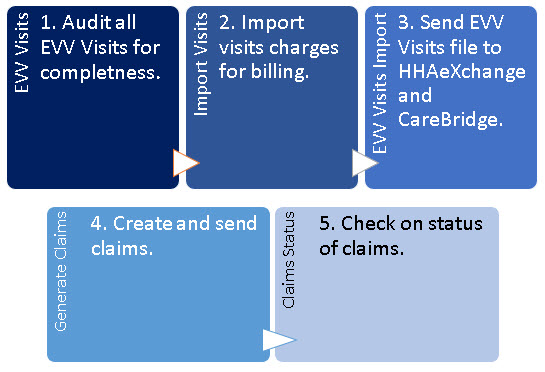
Audit EVV Visits
(HHAeXchange and CareBridge)Monitor EVV Visits Screen: Video EVV Compliance Report: Article Audit your EVV info in EVV Visits. This is what gets sent to HHAeXchange (not charges!). So, if there are any missed visits that were actually done, complete them in EVV Visits. If any staff forgot to clock out of EVV, complete those. Make sure all of your EVV Visit information is cleaned up and complete before you do the process below. As needed, use the following report to verify all EVV Visits are complete and not missing: Reports > Audit > 17.37 EVV Compliance. Select the billing dates and the option for EVV Pre-Billing Audit. Make any corrections before proceeding.
Import Visits to Mark as Ready for Billing
(HHAeXchange and CareBridge)Import Visit Charges: Article This step will take the EVV Visit and add a “charge” to the system for billing. After this process is complete you will be able to create claims and generate the EVV Visit file. 1. Employee Activity > Import Visit Charges. 2. Select the From and Thru dates to match the service dates ready to bill. 3. (Optional) Select the Import Just One Chart# (use this if you already did the main import but found another visit to import). You can also check the box for MCO Only. 4. Make sure bullet for “Round .25” is selected. 5. Click the View Visits button. Review the data that appears to see if any issues are noted. Make changes before proceeding. 6. Click Create Visit Charges to complete this task. We recommend saving this report for your records.
Optional ReportAuthorized Hours Vs Actual Hours: Article You can compare the visit charges that you imported to the number of authorized hours. This report will only work when the following rules have been met: - The patient has an authorization keyed for payer on the EVV Visit.
- The aide care plan is active during the time frame of the report.
- The format of the authorization and report matches, ie. Tracked weekly or monthly.
Prepare and Send the EVV Visits File to HHAeXchangeHHAeXchange will need to receive EVV Visits file for importing into their system and forwarding to Sandata. This process includes MCOs: Amerihealth, Carolina Complete, United Healthcare, Wellcare, ECBI. Note: The HHAeXchange password may need updated every 90 days. You will update your password through HHAeXchange and then update it in Barnestorm, from Barnestorm from Billing > HIPAA Transactions > HHAeXchange/CareBridge > Edit HHAeXchange SFTP Credentials. HHAeXchange PDF with common errors: Click here 1. Go to Billing > HIPAA Transactions > HHAeXchange/CareBridge. Please note that if you have not supplied Barnestorm with your HHAeXchange SFTP credentials, you need to do so before this will work. There is a button on this screen that allow you to change them in Barnestorm. 2. From the HHAeXchange File Create tab - Change the from and thru date to match the dates you've cleaned up and prepared in EVV Visits. The From date that shows up is the date after the thru date of the last file sent to them, so unless you are re-doing a file, it should be correct. 3. Click the Select EVV Visits button. 4. If there are any issues, an error report will pop up. Print or save this so you can solve those issues and send those visits later. Reasons the visit shows up on the error report: 1) the visit was not imported yet. 2) the visit was manually keyed into the system, meaning it is not an EVV Visit. 5. The visits that are ready to send will appear in the main part of the screen. IMPORTANT: Look these over, because if there are issues, you need to go back to EVV Visits and fix them before you complete. the rest of this process! 6. Click the button to Prepare the Import File. What this does is takes all the EVV info on the screen and prepares a file that will go to HHAeXchange in the format they need to import the EVV visits. 7. A pop-up will appear. NOTE: If you click Yes, the file you created will automatically be sent to HHAeXchange right now. If you click No, the file was still created but will not send. So, if you're ready to send the info to HHAeXchange, click Yes. You have completed the process to upload your EVV visits to HHAeXchange. The file gets sent to HHAeXchange automatically. HHAeXchange takes 24-48 hours to process files. They do not provide a response unless there is an error. To check your visits, wait 24-48 hours and then check the HHAeXchange portal.
Resend Visits When They Had Error To re-send visits that had an error on HHAeXchange: 1. View the error: go to Status of HHAeXchange and CareBridge Uploads and then click the file with the error (it will say ERROR on status). You can print or save the status file. VIewing the status file marks the visits that errored so that you can re-send them. 2. Go back to HHAeXchange File Create tab. Pull up the From and Thru dates. 3. Click Prepare the Import File and click Yes to send.
Resend Corrected Visits When Already Sent To re-send visits that were sent incorrectly: 1. Pull up the From and Thru dates 2. Click the Only Previously Sent EVV box. 3. Click Prepare the Import File and click Yes to send.
Status of HHAeXchange and CareBridge Uploads
If a file transmitted shows a Status with ERROR, you can select the file to pull up a report that will give you a brief description of errors related to the visit. At this time, those visits not accepted will be marked as available to process from the HHAeXchange File Create again (without selecting Only Previously Sent EVV). You will want to fix any errors from the report before you attempt to re-send to HHAeXchange or CareBridge.
1. From Billing > HIPAA Transactions > HHAeXchange/CareBridge, go to the Status of HHAeXchange and CareBridge Uploads tab. 2. Select the file with the error status. 3. A report will appear with the errors listed. Optional to print. Click on Close. Attached is a PDF with common errors. 4. At this time any that were not accepted will re-appear on the Select EVV Visits list to resend.
Error Message Agency is not linked with Payer = the enrollment process with the MCO has not been completed yet. HHAeXchange or the MCO would have sent you instructions on how to complete, Barnestorm does not have this information.
Create Report of All Files Sent to HHAX Use the starting transmission date to print a detailed list of EVV Visits sent. The date is based on the transmission date and will include all files starting with that date going forward. At this time any that were not accepted will re-appear on the Select EVV Visits list to resend.
Generate Billing Claims for HHAeXchange
There are three parts of the billing process for MCOs: 1. Sending HHAeXchange the EVV info (required after August 31, 2021)--instructions above. 2. Creating the electronic batch billing claim(s) in Barnestorm for the MCOs). 3. Sending the billing file to Amerihealth, Carolina Complete, United Healthcare, Wellcare; either using Change Healthcare in Barnestorm or sending the billing file to each MCO using their instructions. ______________________________________________________________________ You will use Barnestorm to create electronic claim files for PHP MCOs:
Amerihealth, Carolina Complete, United Healthcare, Wellcare.
You might have to create a new folder in the your local Claims folder (on your computer) called ChangeHC to do so. Create the folder in the same directory where your normal Barnestorm claims go. Example: if your claims go to C:\Barnestorm\Claims, you will create a new folder there that will look like this: C:\Barnestorm\Claims\CHangeHC.
After you create that folder, you will build claims exactly as you always do, for the MCO payers, using All Other Billing. If you have only one PCS NPI, then all the MCO claims can be created at the same time by selecting payers 840,860,870,880,890 (and if you have children billed as 99509:HA, then add payers 841,861,871,881,891).
If you have different NPI numbers for each program, then create separate files for each NPI but putting in the program number.
You will not receive an acknowledgement or response on Change Healthcare. Once it is sent, Barnestorm will contact you if there is an error. Check on the claim status using the MCO portals: Barnestorm will not have the claim status, but the MCOs will. MCOs will pay you directly using the method you set up with them when you registered. ______________________________________________________________________ Providers have reported that United HealthCare and Carolina Complete are paying claims normally, but that Amerihealth and Healthy Blue are much slower.
HHAeXchange has said that they will send Medicaid Managed Care EVV info to MCOs for billing, but so far, that has not happened.
Send Claims Using MCO Portals (HHAeXchange MCOs)
If you do not want to use Barnestorms's Change Healthcare service to send claims, you can use each MCO portal to transmit electronic claim files for MCOs: Amerihealth, Carolina Complete, United Healthcare, Wellcare.
Barnestorm does not have instructions for uploading the claims on each MCO portal: those instructions are included in the billing guide for the MCO, or you can call the MCO for assistance.
Follow the claim status on the MCO portal.
Providers have reported that United HealthCare and Carolina Complete are paying claims normally, but that Amerihealth and Healthy Blue are much slower. MCOs will pay you directly using the method you set up with them when you registered.
Send Claims Using Change HealthCare in Barnestorm
(HHAeXchange MCOs)
Send Claims Through Change HealthCare in Barnestorm: Article You will use Change HealthCare to transmit electronic claim files for MCOs: Amerihealth, Carolina Complete, United Healthcare, Wellcare, ECBI. Note: If you are not using Barnestorm to send claims using Change HealthCare, you will need to use instructions provided to you per each MCO. The following instructions do not apply to those who are not using Barnestorm to transmit claims through Change HealthCare. Billing > HIPAA Transactions > Transmit to Change HealthCare is used to transmit the electronic claim. The left side of this screen are files located on your local machine or server. The right side are files sitting in the SFTP mailbox via Change HealthCare, but you will not receive an acknowledgement or response on Change Healthcare. The purpose of this screen is to select any claims created (left side) and send them to the mailbox at Change HealthCare (right side) to process and send to the appropriate MCO. Once it is sent, Barnestorm will contact you if there is an error. Check on the claims using the MCO portals. MCOs will pay you directly using the method you set up with them when you registered. Follow Claim Status on MCO Portals Once the electronic claims(s) are sent to Change HealthCare, they are processed and sent to the MCO. You will follow the progress of the claim status on the MCO portal. If you have questions about your MCO claims, please contact the MCO. Barnestorm is not involved in MCO claim processing and is unable to give you updates on that. If you need help with the MCO portal, please contact the MCO. Providers have reported that United HealthCare and Carolina Complete are paying claims normally, but that Amerihealth and Healthy Blue are much slower. MCOs will pay you directly using the method you set up with them when you registered.
Prepare and Send the EVV Visits File to CareBridgeCareBridge will need to receive EVV Visits file for Healthy Blue. This is the only MCO using this method. CareBridge PDF with common errors: Click Here Note regarding authorizations: Healthy Blue must monthly authorization keyed in for all patient's listed on the EVV Visit file. If one patient is missing a valid authorization, then check the box 'Exclude Patients With Missing Authorizations' before proceeding with steps. EVV - Add Authorization Dates and Hours (barnestorm.biz) 1. Go to Billing > HIPAA Transactions > HHAeXchange/CareBridge. Click the CareBridge File Create tab at the top. 2. Change the from and thru date to match the dates you've cleaned up and prepared in EVV Visits. 3. Click the Select EVV Visits button. 4. If there are any issues, an error report will pop up. Print or save this so you can solve those issues and send those visits later. 5. The visits that are ready to send will appear in the main part of the screen.
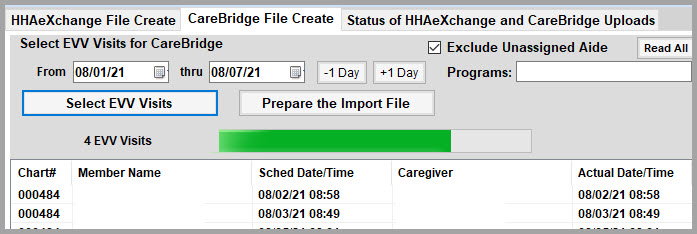
IMPORTANT: Look these over, because if there are issues, you need to go back to EVV Visits and fix them before you complete the rest of this process! 6. Click the button to Prepare the Import File. What this does is takes all the EVV info on the screen and prepares a file that will go to CareBridge in the format they need to import the EVV visits. 7. A pop-up will appear. NOTE: If you click Yes, the file you created will automatically be sent to CareBridge right now. If you click No, the file was still created but will not send. So, if you're ready to send the info to CareBridge, click Yes.
You have complete the process to upload your EVV visits to CareBridge. The file gets sent to CareBridge automatically. CareBridge takes about 3 hours to process files. They provide a response file for each upload.
As of September 1 (in theory), the EVV data sent to CareBridge will be converted to claims and forwarded by them to Healthy Blue. Use Availity to access the Healthy Blue info to see if CareBridge actually created a claim and sent it to Healthy Blue; and if so, get the 835 electronic remittance from Availity (which can take up to 30 days). If EVV data sent to CareBridge does not generate a claim, please contact CareBridge for support. To re-send visits that were sent incorrectly: Pull up the dates, click the Prepare the Import File, click Yes to send (re-sending overwrites, there is no need to mark as replacement). If you need to void a visit because it shouldn't have been sent, pull it up, check the box to Select One Visit to Void, and select the visit by clicking on it. Our understanding is that CareBridge creates the 837 from the EVV Visits you upload and sends them to Healthy Blue. However, this is for providers to verify with CareBridge and Healthy Blue, as Barnestorm is not involved in that part of the process. CareBridge will pay you directly using the method you set up with them when you registered.
NC PCS PHP Medicaid Managed Care Organizations (MCOs) in Barnestorm
Barnestorm has set up new payers for each Medicaid MCO in each of your programs: Amerihealth: 870 adult, 871 child Carolina Complete Health: 890 adult, 891 child Healthy Blue (BCBS): 860 adult, 861 child United Healthcare: 880 adult, 881 child Wellcare: 840 adult, 841 child ECBI: 899
You can run eligibility for your current patients switching to Managed Care, and then add the MCO: -Add the new payer that represents that patient's MCO into Referral > Payers. -Discharge the current Medicaid payer(s) as of June 30, 2021. -Make aide plan changes as noted below to carry these payer changes through to the EVV app. This means that all new visits will be under the new MCO payer in Barnestorm.
For any Medicaid MCO, the first payer on the patient's referral should be the MCO, and that HIC should be their payer ID for the MCO. The second payer should be NC Medicaid and the HIC should be their Medicaid HIC. Some MCOs use the Medicaid HIC and some do not, but NC Medicaid should always be the secondary payer for all Medicaid MCOs--this allows you to check eligibility with NC Tracks through Barnestorm, which allows you to see if & when Medicaid MCOs change--we recommend running eligibility at least once a month for NC Medicaid & MCOs.
Note that the Medicaid HIC goes into HIC# by default. If the MCO does not identify the patient by the Medicaid ID, then you will need to put the MCO number into the HIC # (removing the Medicaid number). Healthy Blue uses the Medicaid HIC#, and you can use the MCO# for the Healthy Blue ID. -------------------------------------------------------------------------------------------------------------
You just need to do a couple of things to manage an MCO transition: 1. Select the patient, go to Referral. 2. Click Authorizations, and add the correct authorization dates for the MCO under that new MCO payer. 3. Click Aide Plan on the main menu. 4. Click the active plan and then click Copy. 5. Make sure the copied plan has a start date of whenever the new MCO is active for that patient. The end date will be the end date of the MCO authorization. Make sure the new MCO payer shows, and that the job code and visit code are correct. Create Schedules and, after that finishes, Save Plan.
Health plansFor health plan questions, or to learn more about covered services, contact the health plan. WellCare (Standard Plan) wellcarenc.com WellCare is offered statewide. UnitedHealthcare Community Plan (Standard Plan) uhccommunityplan.com/nc UnitedHealthcare Community Plan is offered statewide. Healthy Blue (Standard Plan) healthybluenc.com Healthy Blue is offered statewide. AmeriHealth Caritas (Standard Plan) amerihealthcaritasnc.com AmeriHealth Caritas is offered statewide. Carolina Complete Health (Standard Plan) carolinacompletehealth.com Carolina Complete Health is a provider-led entity offered to people who live in these counties: Alamance, Alexander, Anson, Bladen, Brunswick, Cabarrus, Caswell, Catawba, Chatham, Cleveland, Columbus, Cumberland, Durham, Franklin, Gaston, Granville, Harnett, Hoke, Iredell, Johnston, Lee, Lincoln, Mecklenburg, Montgomery, Moore, Nash, New Hanover, Orange, Pender, Person, Richmond, Robeson, Rowan, Sampson, Scotland, Stanly, Union, Vance, Wake, Warren, Wilson. Alliance Health (Tailored Plan) alliancehealthplan.org Alliance Health is available in these counties: Cumberland, Durham, Johnston, Mecklenburg, Orange, Wake. Eastpointe (Tailored Plan) eastpointe.net Eastpointe is available in these counties: Duplin, Edgecombe, Greene, Lenoir, Robeson, Sampson, Scotland, Warren, Wayne, Wilson. Partners Health Management (Tailored Plan) partnersbhm.org Partners Health Management is available in these counties: Burke, Cabarrus, Catawba, Cleveland, Davie, Forsyth, Gaston, Iredell, Lincoln, Rutherford, Stanly, Surry, Union, Yadkin. Sandhills Center (Tailored Plan) sandhillscenter.org Sandhills Center is available in these counties: Anson, Davidson, Guilford, Harnett, Hoke, Lee, Montgomery, Moore, Randolph, Richmond, Rockingham. Trillium Health Resources (Tailored Plan) trilliumhealthresources.org Trillium Health Resources is available in these counties: Beaufort, Bertie, Bladen, Brunswick, Camden, Carteret, Chowan, Columbus, Craven, Currituck, Dare, Gates, Halifax, Hertford, Hyde, Jones, Martin, Nash, New Hanover, Northampton, Onslow, Pamlico, Pasquotank, Pender, Perquimans, Pitt, Tyrrell, Washington. Vaya Health (Tailored Plan) vayahealth.com Vaya Health is available in these counties: Alamance, Alexander, Alleghany, Ashe, Avery, Buncombe, Caldwell, Caswell, Chatham, Cherokee, Clay, Franklin, Graham, Granville, Haywood, Henderson, Jackson, Macon, Madison, McDowell, Mitchell, Person, Polk, Rowan, Stokes, Swain, Transylvania, Vance, Watauga, Wilkes, Yancey. The Eastern Band of Cherokee Indians (EBCI) Tribal Option ebcitribaloption.com The EBCI Tribal Option is for federally recognized tribal members or others who qualify for services through Indian Health Service (IHS) and live in Buncombe, Clay, Cherokee, Graham,Haywood, Henderson, Jackson, Macon, Madison, Swain or Transylvania counties. As a member of the EBCI Tribal Option, you can get services from any NC Medicaid provider. NC Medicaid Direct bit.ly/NCBeneficiaryPortal NC Medicaid Direct is for members who qualify. Other resourcesNC Medicaid Contact Center Phone: 1-888-245-0179 Website: medicaid.ncdhhs.gov/contact NC Medicaid Ombudsman Phone: 1-877-201-3750 Website: ncmedicaidombudsman.org North Carolina Medicaid Application Website: medicaid.ncdhhs.gov/medicaid/get-started/apply-for-medicaid-or-health-choice
Add Your Comments
|
Last Modified:Wednesday, July 19, 2023
Type: INFO
Rated 5 stars based on 1 vote
Article has been viewed 11,075 times.
|