What requirements must be met before sending a RAP for episode dates starting in 2021?
***NOTE: This process applies to Medicare, or any other PPS payer that is marked as using2021 rules (Codes > Payers > Electronic Claims Setup > MA Plan 2021Rules Start Date).
Plan Ahead: We urge HHAs to get in the practice of sending RAPs daily, if you have not already begun to do so. This will be a major change in 2021, and will be a big factor in agency revenue/cashflow. Please inform your staff, including home-billers, of these changes.
In 2021, RAPs will still be required, but there will no longer be an initial RAP payment for the episode. Though, there will no longer be a payment, the RAP is still REQUIRED and must be sent timely(within 5 days) to avoid late penalty. In 2021, RAPs must be filed and ACCEPTED at the MAC within 5 days of the beginning of EVERY 30-day payment period. If it is not accepted within 5 days, the agency will be penalized for every day up until it is received/accepted at the MAC. (There is an example below that shows penalization for a late RAP).
The following requirements must be met prior to sending the Start of Care RAP claim in 2021:
1. The appropriate physician’s written or verbal order that sets out the services required for the initial visit has been received and documented as required; and
2. The initial visit within the 60-daycertification period has been made and the individual is admitted to HH care.
NEW: Even though both 30-day RAP episodes can be billed at the beginning of each 60-day cert period, Barnestorm has chosen to wait until closer to the beginning of each 30-day episode, to avoid placing too much future money into Accounts Receivable. Subsequent RAPs: Since subsequent RAPs can be sent without waiting for the actual first visit, the RAP will be created using day 1 of the 30-day period as the first visit date. That date is no longer required to match the actual first visit date on the EOE claim.
3. At least one diagnosis code on the RAP.(ICD codes on the RAP no longer need to match those on the final.)
Billing of Start of Care RAPs- Changes in Barnestorm for 2021:
Dates used on RAPs: for the first 30-day episode, the RAP uses a start of care visit; this is so it can be sent by day 3, to beat the 5-day window; for following episodes, it uses the 485 and calculates the 30-day intervals.
a. 485: The 485 no longer needs to exist, but if it has been entered, it does not need to be marked as mailed. If it has been printed, then the episodes will be there for the RAP process, or you can still manually create the episodes from the 485 screen. If the Start of Care visit exists, but there is no episode yet, then the RAP process will create it.
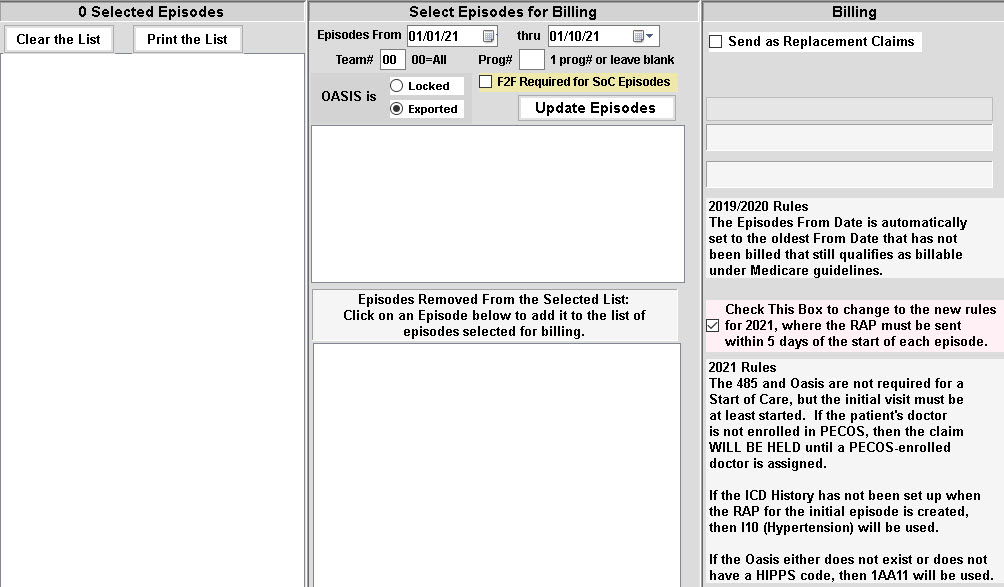
b. OASIS: The OASIS no longer needs to be locked or exported. If the Oasis is complete and has a HIPPS code, that HIPPS will be used. If not, the default HIPPS used will be 1AA11, the bottom of the list. There is a follow-up process that will identify episodes that were sent with that default code and update the episode to the code used on the exported Oasis. The software will adjust the amount in A/R to be correct. The HIPPS code on the EOE is still required to match the HIPPS code that was on the RAP, and the CMS claims processing system will use the M0090 Date of the Exported OASIS to calculate the correct HIPPS code and payment.
c. First Visit of Episode: For the first 30-day episode, a start of care assessment must exist (doesn't have to be complete, and the purpose is just to make sure the patient is actually admitted, and that the admit date matches). For the second 30-day episode and all subsequent episodes, the visit date in the RAP will be the "from date" of the episode.
d. ICD History: The RAP requires at least one ICD code. If the ICD history exists, it will be used. Otherwise, the default ICD code used will be I10 (hypertension, a code that hasn't changed since ICD 10 started). The ICD codes on the EOE will be pulled from the ICD history, not from the RAP.
e. PECOS Enrollment: The Doctor on the RAP needs to be enrolled in PECOS. The RAP will be held at this time if the doctor is not enrolled.
f. RAP Process: On the RAP screen, there is an option to activate the 2021rules before clicking Update Episodes. This will trigger two different processes for creating episodes for active PPS patients. (1)there is a start of care assessment (as per c. above), and there is no episode with that start date (be careful about nursing and therapy start of care episodes agreeing on the start date); or (2) an episode exists with a thru date already ended or will end in the next 3 days, and there is no existing 202130-day episode.
Reason for Sending RAPs ASAP
The RAP also serves a greater role for the Medicare program, by establishing your agency as the beneficiary’s primary HHA in the Common Working File. Therefore, to not only avoid late penalties, it is also important to establish your agency as primary to avoid possible payment losses/delays. We recommend doing the RAP process daily starting Jan 1, and pay close attention on Fridays to make sure none slip by that would be due on Sun ( or a Mon holiday), to avoid late penalties.
Penalty for Sending Late RAP: Scenario
30-DAY PAYMENT PERIOD 01/03/21 –02/01/21:
RAP accepted at MAC on 01/20/21,
The HIPPS Code value is $2,800,
When final is paid, the agency will receive the following payment: – $2,800 divided by 30 = $93.33 per day,
$93.33 X 17 days = $1,586.67 ( In this scenario the RAP was 17 days late),
$2,800 - $1,586.67 = $1,213.33(payment the agency will receive, minus the late penalty)
For purposes of determining if a “no-pay” RAP is timely-filed, the no-pay RAP must be submitted within five calendar days after the start of each 30-day period of care. For example, if the start of care for the first 30-day period is Jan. 3, then the no-pay RAP would be considered timely-filed if it is submitted on or before Jan. 8.
In the event that the no-pay RAP is not timely-filed, CMS will calculate the one-thirtieth penalty from the first day of that 30-day period. Using the previous example, the penalty calculation would begin on Jan. 3 — and not on Jan. 9, the first day after an agency misses the filing deadline.
Please view CMS article regarding: PENALTY FOR DELAYEDREQUEST FOR ANTICIPATED PAYMENT (RAP)SUBMISSION.
BARNESTORM: Here's the 2021 RAP process:
When a Start of Care assessment is found (does not need to be completed or locked) for Medicare, or another PPS payer that is marked as using2021 rules, then if no episode has yet been created (by printing the 485), then it is created in PPS Tracking - a report will generate showing RAPs added. The first report will be longer than the typical process to add 2nd 30-day episodes.
When RAP claims generate:
If there is no Oasis with a HIPPS code, mark the episode with document id = @@ and use 1AA11 as the HIPPS;
If there is no ICD history, use I10 as the primary ICD code;
If there is no doctor assigned to the patient, or if that doctor is not enrolled in PECOS, the episode will be held.
For all episodes beyond the Start of Care:
When the most recent episode Thru date will end in 3 days or has already ended, create the next episode, and then follow the same sequence as above.
This should prevent any late episodes, except for at least 2possible reasons: 1. The start of care assessment has the wrong date, so the first episode was created and sent with the wrong date; 2. The power and internet are out for an extended period. The Edit PPS Episodes screen will have a checkbox for 2021 Late RAP Info that will put in the KX modifier and the comments for the reason.
The 14.03 report will have a new tab for 2021 RAPs that will update the episodes that were sent with document id @@ and locate a correctly dated and exported Oasis with a HIPPS code, checks to make sure the 485 has been mailed and returned, and update the episode for tracking, and update the $Amount in Accounts Receivable. This must be done before those episodes can have an EOE claim created (or to show up on the EOE Error list).
The EOE process will be the same. It will perform several validations:
Verify that the episode from date matches a 485 from date, or matches a 485 from date + 30 days
Verify that the 485 has been mailed and returned
Verify the existence of ICD codes dated on or before the episode from date (clinical group edit takes place when the primary code is entered on the Icd History screen)
Verify that all physician orders that apply to the 30-day period have been returned
For SOC episodes, verify that the Face-to-face documentation is marked completed
Verify that the episode Oasis still exists, still has the same M0100 RFA, the same M0090 date, and has not been inactivated
For agencies in RCD states that have chosen pre-claim review, make sure the UTN is there
FAQ
Q: Where do I go to check for RAPs every day to make sure I don't miss any?
A: The RAP screen itself is the best to start with, because it now creates any missing episodes based on episode dates and start of care assessments. Then you can use the 14.03 reports to track them.
***More changes in 2022: RAP now NOA. Click here for those changes.