VA Home Health Services *may* be requiring that billing be done in 60 day episodes and bill like Medicare. The effective date for this transition is October 1, 2014. We are not clear on how they want billing completed for patients who were active prior to October 1, 2014, crossing into the new billing rules. This new rule appears for agencies that do not have a contract with VA - See the attached document.
Tips on how to proceed:
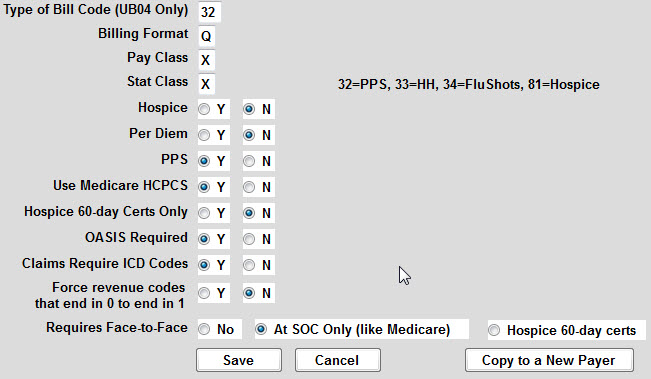
Create a new payer for VA PPS from Codes > Program Related Codes > Payer Codes (see screen shot below on how this should look).
For each current patient that was admitted on or after October 1, 2014, assign this new payer to the Referral > Payer screen.
For patients admitted prior to October 1, 2014, we believe that they will need this new payer only if they have a new authorization on or after October 1, 2014. This part they do not make clear.These patient’s will only need the new payer added to the Referral >Payer screen as needed.
If you need to back track and change visit entries from the old VA payer code to the new VA PPS payer code, use Barnestorm Office >Employee Activity > Fix Payer/JobCd/Chart# to update the payers (see article attached as need for more info on this feature).
Here is an excerpt from the National Association for Home Care and Hospice website:
“The VA also clarified that for episodes beginning on or after October 1, 2014, the VA will require an OASIS and HIPPS code on claims. Initially, claims will not be rejected if the HIPPS code is not present, and will be paid at the current VA fee amount.”
http://www.nahc.org/NAHCReport/nr141028_1/