The purpose of this report is to help you keep track of your billing, and any claim denials. In one location, you can document any communications with the patient and/or insurance company, pertaining to any and all claims for your patient. The process is very simple. Here's how:
To access this report, go to Barnestorm Office > Billing > Other > Track Unpaid Billing.
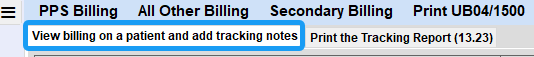
The screen that appears will have 2 tab options: 1. View billing on a patient and add tracking notes, and 2. Print the Tracking Report (13.23). Follow these instructions for Tab 1. Then proceed to Tab 2 to print the report.
View Billing on a Patient and Add Tracking Notes: Tab 1
1. Enter the patient’s chart number or name. As needed, select the Active bullet or select the number of days since discharge. If the patient does not appear, or if no information appears on the screen, this means no billing has been generated for the patient.
2. If the patient has multiple payers, you will need to select the applicable payer from the listing that appears. A grid will then appear at the bottom of the screen.
3. This grid will show you the From and Thru dates, batch claim number (file name) of the claim, the date of transmission, the amount billed, the balance, the status of the claim and the next follow-up date assigned.
The $Amount column reflects the total amount on the claim, which does not match the Amount Billed in the A/R.
The $Balance column reflects the Balance from the A/R.
Optional ways to filter the data that appears in the Grid:
1. From / Thru Dates: The From Date will default to the patient's admit date. The Thru Date will either be the current date, if the patient is active; or the patient's discharged date if the patient has been discharged. You can leave as is, to pull all dates of service that have been billed, or you can modify to the specific dates you need. Use the +1mo or -1mo, and the grid will automatically update. If you manually change the date, you will need to reselect the Payer to refresh the grid.
2. Ignore RAPs and/or Unpaid Claims Only: Select either bullet to ignore RAPs/NOAs; or select the option to only view the unpaid claims.
Enter Notes and Keep Track of Billing:
1. Once you have the patient pulled up, select the billing cycle in the grid to pull up the notes screen.
2. A new screen will appear, which allows you to keep a running commentary of notes regarding the patient’s account and/or to keep track of phone calls.
3. Use the Next Follow-up Date to remind yourself of when you want to take the next action on that claim. This can be seen in the last column of the grid as well as on the report. See "Printing the Report."
4. Use the Add Date/Time Stamp to the text tab to timestamp the date and time you entered your notes.
5. Use the Status of this Claim section to mark/change the status of the claim. This is where you can mark the claim as New, In Progress, Completed, Uncollectable, RAP, RAP Paid, EOE or EOE Paid. This will also show in the grid and on the report. See "Printing the Report."
6. Click on Save when finished. This takes you back to the list of claims. Follow the next steps to print the report.
NOTE: If you enter notes in error, you can delete the tracking notes. Select the line item, from the Grid, by doing a right-click. You will receive a popup: "Are you sure you want to delete the billing tracking details for this entry?" Select Yes to delete; or No to remove the popup. IMPORTANT: Selecting Yes, will remove the tracking details. Be certain you want to remove the data, as this information will be removed from the system.
Printing the Tracking Report (13.23): Tab 2
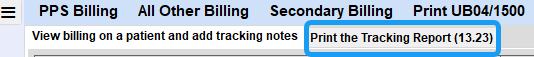
1. Click Print the Tracking Report (13.23) tab.
2. Program(s) /Payer(s) = Filter report by entering program or payer number(s). Or leave blank to search all.
3. One Chart# = Put in a specific chart number, or leave blank to search all. If you type in a chart number, but then decide to search all, click the Clear the Chart# so all patients with selected program and payer print option to clear that chart#.
4. From and Thru dates = These will select the billing based on the claim's From date. Or select the Find Oldest Unpaid A/R button to adjust the from and thru dates. You can use the +1mo or -1mo options to change the month view.
5. Click the 13.23 Print Billing Tracking button to view all claims, based on the criteria above. This report will show the billing info for each claim by program/payer and then by patient.
Optional ways to filter the data that displays in the report:
1. Unpaid Claims Only - This option will generate a listing of all unpaid claims where you have started tracking the claim on this screen.
2. Newest Claim Only - This option will generate a listing of all claims marked with the status of "New", where you have started tracking the claim on this screen.
3. Claims with Follow Up Only - This option will generate a listing of all claims, where you have indicated follow-up is needed, where you have started tracking the claim on this screen. This listing will also include all comments entered regarding the status of the claim.
4. Ignore RAPs - This option will ignore all RAPs/NOA where you have started tracking the claim on this screen.
Make any additional selections, then click the 13.23 Print Billing Tracking button to print.