Eligibility Verifications for Medicaid (270 / 271)
NC Medicaid Direct (NCTracks) – Process Flow
YOU ARE HERE
Verify Eligibility
→
Visits Audited / Imported
→
Claims Created
→
Transmit to NCTracks
→
Post Remit File
Overview
Use this workflow to verify Medicaid eligibility before billing. The process includes creating eligibility requests (270),transmitting them to NCTracks, receiving responses (271), and reviewing results. This should be done at the beginning of each month and prior to new member service rendered.
Primary Locations - Billing > Other > Create Eligibility Verifications
- Billing > HIPAA Transactions > Transmit to NC Medicaid
1) Create Medicaid Eligibility Verifications (file type 270)
- Go to Billing > Other > Create Eligibility Verifications.
- Review Eligibility Dates (defaults to current month; adjust as needed).
- Patients discharged before or admitted after the range are excluded.
- Future dates are not allowed.
- Select a Medicaid payer from the left panel.
- Configure options on the right:
- Only one NPI can be used at a time.
- Check Include ALL Medicaid (CAP+PCS+HH+MCO+LME) Patients.
- Optional: Include Referred but Not Admitted or Select All PCS.
- Click Create Eligibility File.
- Optional: Print Patients in Eligibility Batch.
- Click anywhere to return and repeat for additional NPIs or payers.
Advanced: Auto-Send (Auto-Billing)
If enrolled in auto-billing and Auto-Send is checked, the eligibility file transmits to NCTracksimmediately after clicking Create Eligibility File.
2) Transmit Eligibility Files to NCTracks (file type 270)
- Go to Billing > HIPAA Transactions > Transmit to NC Medicaid.
- Wait to establish a connection.
- Check the Eligibility bullet.
- Select the eligibility file (270) from the Local (left) panel.
- Use All Files if you do not see the file.
- Click Send and watch the file status box appear, then click Refresh File List.
- An up arrow next to the file name indicates the file was sent.
3) Receive Eligibility Response (file type 271)
- Return to Transmit to NC Medicaid 1-2 hours later.
- In the NCTracks Mailbox (right panel), review available response files.
- Select the 271 file(s) and click Receive.
- Receiving the same file more than once will not create issues.
- You may need to widen the column for file name to view file type.
- If successful, the 270 file on the left side will show a green checkmark, indicating NCTracks received the file.
4) Understand Eligibility Results
- Go to Billing > Other > Print Eligibility Verifications.
- Select the File Name from the right side then click Print Eligibility Verifications.
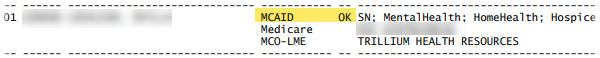
- Program CAPDA or MCAID with a status of OK means Medicaid direct coverage is active for the requested dates.
- Program MQBB with a status of MQ means Medicaid pays the Medicare Part B Premium, and that services are not covered by Medicaid. CAP services cannot be billed to Medicaid.
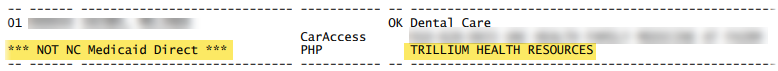
- ***NOT NC Medicaid Direct*** means the patient has an active account with the provider listed beside PHP, ex. United HealthCare or Trillium Health Resources.
- Inactive means that the patient does not have Medicaid for the selected month of the report.
- 72 Invalid/Missing Subscriber/Insured ID means that the Medicaid HIC# was not found, or the name or birth date does not match NCTracks records.
- Pvt Insurance will let you know if the patient also has a private insurance policy. Nothing else needs done unless the patient is being billed for skilled services, which may require a denial from the insurance first.
- Medicare Missing D9 - NC Only, this report checks for Medicare conditions requiring special billing codes. If the patient has Medicare but is not homebound, then you have to bill Medicaid and use the D9 condition code on the claim to indicate that Medicare is not the primary payer for that service.
Example of Medicaid Direct, not PHP/LME.
Example of PHP/LME, not Medicaid Direct.